
The Eye Exam for Patients with Diabetes HEDIS® measure changed from a hybrid measure to an administrative measure. This means health plans will rely primarily on administrative claims data—rather than manual chart review—to determine whether diabetic patients received their annual eye exam.

To more efficiently process a prior authorization request, some of the clinical information that may be helpful in processing a request is listed below.

Updated prior authorization forms are now available.

While CPTII codes are not required for reimbursement, they CAN benefit your practice and your patients. Here’s how.

Here are tips to help with utilization management processing.
Have you ever struggled to find a Davis Vision or Superior Vision member’s eligibility? Before you turn that member away, allow us to assist you and ease frustrations while also improving your member’s experience.
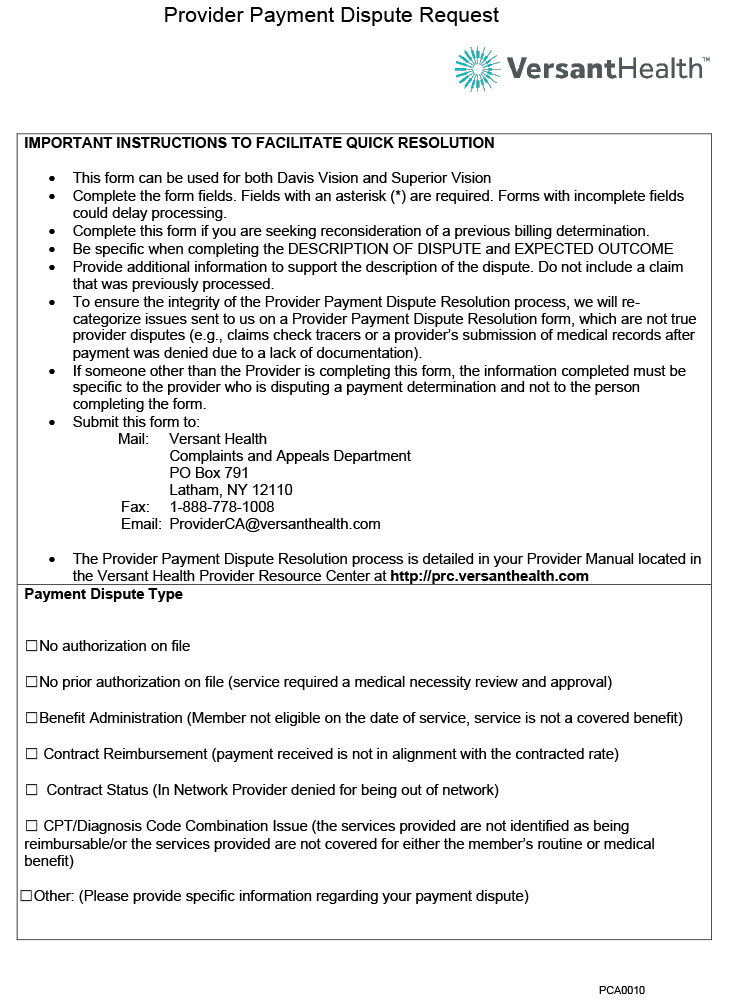
To facilitate a quick resolution, please use this form which can be applied to both Davis Vision and Superior Vision.

The Superior Vision claims mailing address has changed, and all paper claims should be sent to this updates address.

The Utilization Management department has created a short 2 ½ minute video with helpful tips to support a seamless process for submission of prior authorization requests

Complete this form if you are seeking reconsideration of a previous billing determination.